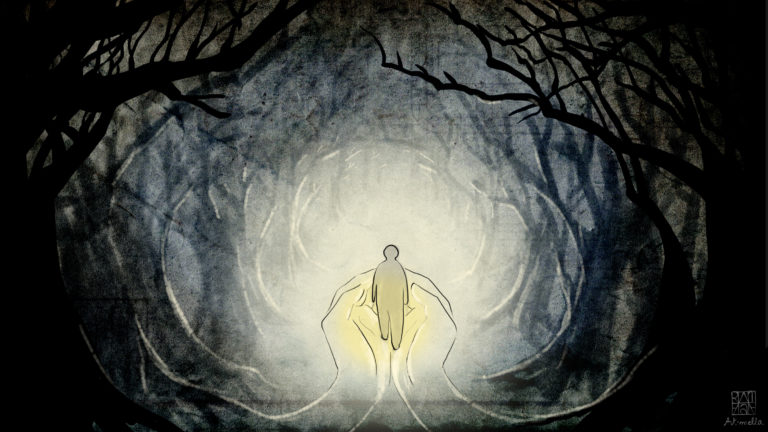
The Gift of a Comforted Transition
- Jocelyn Yerxa
- May 17, 2023
- 6 min read
I am a child of aging parents (an 80-year old mother and recently deceased father). I am also a pet lover and have had a number of pets throughout my childhood and adult life. I am a professional (public servant, actually) who has worked on aging issues for almost 15 years. Most recently, I have become a death doula candidate with Home Hospice Association. All of these things are connected and important parts of my life journey that have brought me to care deeply about home hospice and palliative care options. The perspectives are mine alone, although I hope others will agree (or at the very least consider them with an open mind and heart).

2020 was a big year for me (for many people, I would imagine). It's the year my dad and cat of 16 years both died. It's the year that COVID-19 shaped a major change in life for the world and brought many of us to think about dying and death. I remember watching the Johns Hopkins Data Dashboard and seeing the climbing number of COVID infections and deaths. Every news channel had daily updates government leaders on infections and deaths most of the year. Dying and death were everywhere. aIn my life I had the privilege to journey with two souls I loved deeply to their transition out of this life.
The experience with my dad’s end of life happened at the beginning of the COVID-19 pandemic. We knew my dad did not have long to live in the fall of 2019. We supported him and did all the things he wanted to take care of (mostly selling property) before he died so my mom would not have to worry about them. My sister and I spent the Christmas holiday in Florida emptying and packing up their home so that it could be sold. In February 2020, things had taken a turn for my dad, and he was really only up and out of bed for a few hours a day. At the beginning of March, he had a fall and my mom was at her wits end with different opinions from multiple care providers and no help with respite care. There was a day when I talked to my mom, and I could tell she could not handle what was happening. So after work, I packed my bags and animals to go live with them until we could figure out a plan to support both of them.
I don’t think I was there for 24 hours when my dad said to me, “Jocelyn, you have to figure out this Medical Assistance in Dying thing before it is too late for me to make the decision.” In that moment and over the next short while, my experience in providing feedback and policy advice on the legislation became very personal How the legislation actually works in reality became a real-life experience for me and my family. For the most part, I had deep gratitude and appreciation for my dad being able to make the choice and for everyone that helped my family during that time…but I shouldn’t jump too far ahead.
Let me back up a little bit. My dad's diagnosis of Leukemia came after quite a long wait. There were doctors on vacation and a focus on what they thought was going on (heart or liver) that meant they hadn’t considered it could be something. It was his cardiologists looking at some test results while his gastroenterologist was on vacation who noticed something other than heart or liver issues were happening. After that, things moved quickly. My dad was cared for by a hematologist-oncologist and started chemotherapy. It was after maybe his second or third chemotherapy session that a palliative team - nurse and doctor - were assigned. They saw him at home and talked to him about all sorts of care needs. I can remember that being a “wake-up call” for me.
It was the first time I thought, “maybe my dad is not going to make it through this illness.”
In fact, the differences in how the hematologist-oncologist and palliative team approached what was happening with my dad caused a lot of conflicting messages for my mom, who was just trying to manage what was a complete change in life for her. For patients, it is really important for meand why I chose to become a death doula. and why I chose to become a death doula. dical teams to work as an integrated unit. I can’t understand why the palliative team and oncology teams weren’t connected. Why wasn’t there a professional connection that allowed everyone to assess the situation and for them to talk to my dad about what he wanted and my mom about what she needed?! My mom’s role with my dad was equally as important, and it was much more emotionally charged for her. She was losing her partner of more than 50 years. Her world was turning upside down.
My dad was fortunate to have a peaceful death in hospital surrounded by his wife, children, and even my dog. It was a gift that happened four days before notice of the first COVID-19 lockdown in Nova Scotia. Because of the lockdown we were unable to have the celebration of life we intended. I stayed with my mom for four and half months. I was able to work from home due to COVID, so it worked out well. Her grief and my grief were very different and the stress of COVID added another layer that was really challenging. It was about four to six weeks after my dad’s death that my mom got her first grief package from our health authority. It was pretty much the only support she got at that time. It was a pamphlet and FAQ sheets. (I think there was a place that she could call if she wanted to join a grief support group, but she never called, so I am not 100% sure.) She got the second package close to the one-year anniversary. My sisters and I encouraged my mom to get grief counselling and she did go a few times. But really, the support for her grief process was very minimal.
For me, in the fall of that year, my 16-year-old cat also came to the end of her life. I had spoken to my vet about her coming close to the end of her life at our last annual checkup not long before. He said, “you will know.” And I did know. I had conversations with friends and family that I knew the time was here and what I should do. Many people said to take her to the vet. My thought was if I do that, they will either try to convince me to “save” her, or they will want to euthanize her. She wasn’t in pain, and I thought I needed to be with her while she made her transition.
I spent a whole day and night lying in bed with her. I wasn’t sure if I was going to be able to do it, but having just had the experience with my dad, I didn’t want to drag her to a vet office and have her take her last breaths there. It was the most precious time and felt like a gift. It was pouring rain and freezing cold that day. But I went outside crying my eyes out and dug a hole to put her to rest close to home. It's really comforting to know she is there.
Both of these experiences were really the foundation of me thinking I wanted to take HHA’s death doula certificate program. I could see the sacred nature of journeying with people and animals at the end of their life. I could see how it can be scary, but I also believe it can give comfort to individuals who wish to die at home, surrounded by love. For me, the option for home hospice and supports beyond medical intervention are central to improving palliative care in our country. I hope that my work as a death doula will be a part of making palliative care better.
Anyone interested in becoming a death doula can register for HHA's Death Doula certificate program here. The next available training weekend is June 2-4, 2023.
---
Jocelyn Yerxa is a death doula candidate with Home Hospice Association.




Comments